In the global tussle to subjugate humanity’s colossal foe Covid-19, one thing that is eagerly sought after by everyone is immunity against novel Coronavirus. This immunity can either be achieved naturally by getting exposed, infected and recovered from the virus or through mass vaccination programmes. Among many medical terminologies that are colloquially used these days, herd immunity is one of them. Is herd immunity the ultimate weapon against novel Coronavirus? In the long term-yes however in the current scenario it is highly unpredictable and hypothetical to suggest that herd immunity can protect against Covid-19. Genetic instability (high frequency of mutations) is an inexorable trait of viruses. And it is not uncommon for an attenuated virus (vaccine) to undergo recombination with the circulating virus and take a mosaic form. That said, it is an unsubstantiated forewarning and upcoming researches will clear the clouds hopefully. Let us understand what is herd immunity, how it works, is herd immunity the ultimate weapon against novel Coronavirus and what is the current status of Coronavirus vaccines all over the world.
What is herd immunity?
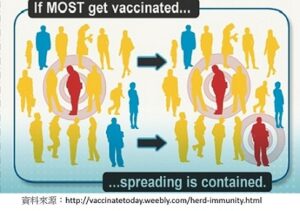
Herd immunity is a form of immunity that an individual gets against an infectious disease when he is surrounded by a group of individuals (herd) who are either vaccinated or have naturally developed antibodies against the pathogen. This means few individuals are effortlessly benefited by living in a community where a significant proportion of people are immune to the infectious disease.
This herd (the immune population of the community) provides indirect immunity even to those who are yet not immune against the pathogen simply by coming in contact with them. Therefore it is also called contact immunity.
The concept of herd immunity is notably beneficial for the vulnerable (at-risk) population of the community (immuno-compromised individuals, pregnant women, children, elderly, those who are not eligible to receive vaccines like cancer patients, those with chronic disease such as diabetes, chronic kidney disease).
How does one develop immunity against an infectious disease?
Two ways of developing immunity against an infectious disease are –
- Getting vaccinated or
- Getting exposed, infected and recovering from the pathogen.
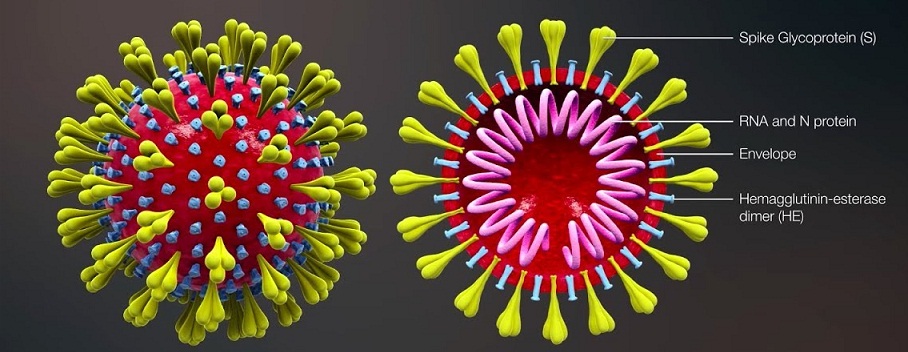
Both the ways induce artificial immunity against an infectious disease by administering the attenuated form of the pathogen (antigen) in the susceptible host. This triggers protective antibody formation (immune response) in the body of the susceptible host. Vaccination is undoubtedly the safest way to get immunity.
So does that mean vaccination and herd immunity provide the same level of protection against disease? No, certainly not. Immunity with vaccination is higher than that with herd immunity. So, it cannot be a replacement to vaccination. Herd immunity is ultimately the very basis of any vaccination programme. However, trying to win the battle against a pandemic like Covid-19 solely on the basis of herd immunity (especially without any containment measures) would be a catastrophic and insensitive approach.
How does Herd immunity work?
The vulnerable members of the community receive protection under the aegis of herd immunity. Let us understand how does herd immunity work?
When a significant proportion of the population is immunized against the infectious disease, it becomes difficult for the pathogen to spread to the susceptible individuals who are yet not immune against the pathogen. Subsequently, the disease slows down both due to the direct effect of immunization and the indirect effect of herd immunity.
For example in the past, polio virus was eradicated with mass vaccination that generated herd immunity. Virus transmission was contained for small pox, 2013 measles outbreak in Wales on similar lines.
The level of herd immunity in a population can be assessed by the reduction in the magnitude of the Basic Reproduction Number of the virus (R0 or R naught).
Is Herd Immunity the ultimate weapon against novel Coronavirus?
Indeed yes. However the vaccine against novel Coronavirus is minimum an year away to hit the markets if we take the best case scenario. Then the only option left to combat Covid-19 in the near future is through herd immunity. However recently WHO presented an unflattering report suggesting that only 2-3% of the world population has been infected with Coronavirus. That’s a pocket-sized proportion globally. Meaning barely 2-3% of the global population has yet acquired antibodies against Coronavirus1.
Now the most important question that arises is what proportion of the population should get infected (rather immunized) with the virus to achieve herd immunity? That means, we need to know the herd immunity threshold. Herd immunity Threshold is defined as the minimum proportion of the population to be immunized to eliminate the infection. This threshold depends largely on the type of infection, location, population density.2 For example, during the H1N1 pandemic 20094, the basic Reproduction Number (R0) was between 2 and 3 and the herd immunity threshold needed was 70%. Whereas measles outbreak in 2013 in Wales, the herd immunity threshold needed was 93-95%. R0 for measles was found to be 12-18 which was unusually high compared to Covid-19. According to an ICMR study6, R0 for novel Coronavirus infection is calculated to be between 2 and 4. The formula to calculate herd immunity threshold is R0– 1/R0. Consequently, immunization coverage of minimum 50%-75% of the Indian population will be necessary to achieve herd immunity. This would amount to approximately 0.6 to 1 billion of the Indian population (Population of India at present is 1.38 billion).
It is difficult to establish herd immunity in cases where the virus is extremely contagious and where high level of population immunity is required.3 Undeniably, we need mass vaccination to achieve such a high herd immunity threshold.
Current status of vaccine production all over the world
At the moment we do not have vaccine to fight the current covid-19 pandemic and majority of people globally are still vulnerable to this disease. However researches are going on at meteoric pace to develop vaccine against novel Coronavirus. Currently, 7 research groups are the pacesetters who have embarked upon human clinical trials, according to WHO research database7.
Vaccine development is an extensive process involving various stages. It typically begins with pre-clinical or animal testing before stepping towards clinical trials or human testing. Human testing takes place in three phases. Clinical trials do not begin unless enough safety data is collected to make plausible decisions about exposing humans to the investigational vaccine. The patient population in each phase of clinical trial keeps increasing. Phase I are small scale safety studies with as few as 20 to 100 healthy participants. Phase II involves several 100 participants and evaluates vaccine efficacy. And phase III being the largest phase includes 1000s of patients at multiple research centers to further assess the efficacy of the investigational vaccine. At the end of phase III, a formal request is sought from the regulatory authorities to be allowed to market the vaccine. Normally, the vaccine development process may take several years (4-5 years or more). However, these phases simply serve as milestones in the vaccine development process and are not necessarily distinct. In frenzied situations like current covid-19 pandemic, the process can be expedited and sometimes phase II and III can be combined for quicker results. While researchers are making a beeline to accelerate the process, it is imperative not to compromise on authentic data collection.
The 7 trailblazer pharmaceutical companies7 who are darting for a vaccine against Coronavirus are in various phases of vaccine development process. Some are in phase I and some in phase II and one of them about to begin phase III. Amidst all this, expert estimates says vaccine is minimum a year away to hit the markets and that’s already the fastest they can make.
Additionally there are 80 research groups globally listed at WHO database who are in the pre-clinical stage of vaccine development. Around 6 organizations from India (Zydus Cadila, Serum Institute, Biological E, Bharat Biotech, Indian Immunologicals, and Mynvax ) have begun pre-clinical studies. Out of which 2 organizations (Zydus cadila, Ahmedabad and Serum Institute of India, Pune) are listed in the WHO database5.
As these clinical trials all over the world would be enrolling large number of human volunteers at various research centers it will ultimately contribute to herd immunity however small contribution it may be. Till the time we have all the above arrangements in place, we need to follow the non-pharmaceutical measures strictly such as social distancing, isolation of symptomatic cases, no unnecessary travel, return to work of recovered Covid-19 cases, kindergarten and primary school closure and liberal utilization of personal protective measures (wearing masks and hand hygiene), if we wish to start our normal lives soon.
The only worry is even if all the non pharmaceutical measures are effective in slowing down the transmission of the virus, the pandemic will be contained only when enough of the population has been infected to reach herd immunity (R0 <1). And in the absence of herd immunity, when the lockdown will be uplifted, looking at the itinerant nature of virus the transmission will resume.
References
- WHO warns that few have developed antibodies to Covid-19. https://www.theguardian.com/society/2020/apr/20/studies-suggest-very-few-have-had-covid-19-without-symptoms
- Lahariya C. Vaccine epidemiology: A review. J Family Med Prim Care. 2016;5(1):7–15. doi:10.4103/2249-4863.184616. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4943153/
- Black FL. The role of herd immunity in control of measles. Yale J Biol Med. 1982;55(3-4):351–360. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2596463/
- Mathematical modelling of the pandemic H1N1 2009. Weekly Epidemiological Record. WHO. No.34, 2009,84,341-352. https://www.who.int/wer/2009/wer8434.pdf
- https://www.livemint.com/news/india/covid-19-six-indian-companies-working-on-coronavirus-vaccine-11587016987400.html
- Mandal S, Bhatnagar T, Arinaminpathy N, Agarwal A, Chowdhury A, Murhekar M, Gangakhedkar RR, Sarkar S. Prudent public health intervention strategies to control the coronavirus disease 2019 transmission in India: A mathematical model-based approach. Indian J Med Res 2020;151:190-9. http://www.ijmr.org.in/text.asp?2020/151/2/190/281325
- Draft landscape of COVID 19 candidate vaccines. WHO. 30 April, 2020. https://www.who.int/who-documents-detail/draft-landscape-of-covid-19-candidate-vaccines




Recent Comments