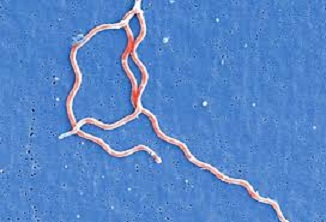
Lyme disease is a bacterial infection spread among humans by the bite of infected deer ticks (belonging to the family Ixodidae). The tick gets infected by feeding on deer or mice already infected with the bacteria Borrelia burgdorferi. So, not each tick bite ends up in Lyme disease. One can get Lyme disease only if the tick had bitten an infected animal previously. It usually affects multiple organs of our body like skin, muscles, joints, nervous system and heart.
According to CDC (Centers for Disease Control and Prevention), Lyme disease is the most prevalent of the tick transmitted infections in U.S. In an intensive analysis of data reported to the National Notifiable Diseases Surveillance System for sixteen vectorborne diseases, Lyme disease was sixth most commonly reported notifiable infectious disease credited with 82% of the tick-borne disease reports throughout 2004-20161. CDC research indicates over 300,000 cases are diagnosed and treated each year in U.S with total cost of Lyme disease testing at about $492 million2.
Prevalence of Lyme disease is seen more in central, eastern, and northern Europe and in parts of Asia, U.S. and Canada.
How are humans infected with Lyme disease?

Humans are infected with Lyme disease from a tick bite on the skin. Infection occurs only if the tick carrying bacteria (Borrelia burgdorferi) remains attached to the host skin for at least 24 hours. More is the time of skin exposure to tick, more the risk of infection. Risk will increase to 100% if the tick remains on the skin for three days. Therefore the most effective prevention of Lyme disease is early detection and removal of the ticks from the skin. How to remove tick from the skin? Simply hold it with tweezers and pull them away from skin. Do that gently so any a part of the tick isn’t left within the skin.
Ticks are found throughout the year however cases of Lyme disease are frequently seen during spring and summer season when the nymph (nascent) ticks are most active and almost undetectable due to their smaller size (poppy seed size).
Transmission of Lyme disease cannot ensue through water, food, air or through bite of any other insects like mosquito or lice.
What are the symptoms of Lyme disease?
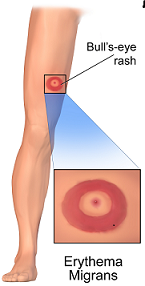
- One of the distinct noticeable symptoms of Lyme disease is appearance of a rash that begins as a tiny red spot (called Erythema Migrans) at the positioning of tick bite. The rash could take from three days up to three months to appear from the time of tick bite and could last for many weeks. The rash gets larger in size (approximately 5 cm in diameter) in consequent days with central clearing giving it a Bull’s eye on dartboard appearance.
- Other concomitant flu-like symptoms such as fever, fatigue, headache, muscle and joint pains, neck pain or stiffness and swollen lymph nodes can also be present.
Why is prompt treatment important in Lyme disease?
It has been observed that if antibiotic therapy is given at the stage of Erythema Migrans, the treatment is curative in 99% of the cases3. If the disease is left untreated at this stage and the treatment is delayed, then it may progress to the disseminated stage and affect other organs of the body such as muscles & joints, central nervous system and heart. This development may take from 6 months to a year.
The disseminated stage of Lyme disease include the following symptoms
Muscles and Joints
- Inflammatory arthritis. Migratory pains and swelling in one or more joints. Large joints particularly knee joint is commonly affected.
- If the symptoms persist chronically, the late stage Lyme disease symptoms appear such as chronic arthritis with joint edema and recurrent inflammatory episodes.
Central nervous system
- Meningitis characterized by severe headache & stiff neck.
- Cranial nerve palsies such as Bell’s palsy (face drooping) characterized by paralysis of one or both sides of the face.
- Radicular shooting pains interfering with night sleep arising from the bacterial invasion of the cranial nerve roots.
- If the symptoms persist inveterately, it may slowly progress to cognitive and memory impairment in the late stage.
Heart
- May get affected after several weeks of infection presenting symptoms of heart blockage, pericarditis, dizziness and palpitations which may get resolved spontaneously in large number of cases.
- Eye symptoms such as keratitis or uveitis
Even though Lyme disease is responsive to antibiotic treatment, inflammatory reactions persist in some individuals after the treatment leading to chronic symptoms4.
Prompt diagnosis and early treatment could scale back the chance of additional symptom development and progression to the disseminated stage.
How is the diagnosis of Lyme disease confirmed?
Diagnosis of Lyme disease is based on history of tick bite and the typical tell-tale symptoms of Lyme disease (Erythema Migrans). According to National Institute of Clinical Excellence (NICE), in cases where characteristic skin rash is present, diagnosis of Lyme disease can be confirmed without the need for blood tests.
Anti Bb antibodies (Lyme disease antibodies) take approximately 2 -4 weeks to rise to detectable levels after the initial tick bite. The antibodies reach to its peak 6-8 weeks after infection.
The typical skin rash of Lyme disease (Erythema Migrans) appears only in two-third of the cases and takes 3-30 days to present after tick bite. The rash gets larger in size (approximately 5 cm in diameter) in subsequent days with central clearing giving it a Bull’s eye on dartboard appearance. This skin rash appears much before antibodies appear in blood therefore patients presenting with the skin rash may have negative blood test results. So, diagnosis of Lyme disease can be confirmed if the characteristic erythema migrans is present and no need to wait for the blood tests. Further, the rash is a more reliable sign out of the two.
In cases where the rash does not appear, lab tests are advised. CDC suggests a two step blood tests that includes high sensitivity ELISA test followed by more specific confirmatory Western Blot Assay to confirm the disease.
How can Lyme disease be prevented?
Lyme disease can be prevented by following simple precautions like:

- Avoid bushy, woody and grassy areas whereever contact with ticks is more likely as these are typical tick habitats, particularly in spring and summer season.
- Keep your body covered when outdoors. Wear full pants and long sleeves.
- Common body parts where ticks settle are groins, back of knee, hairline and armpits.
- Be aware and check for ticks regularly when outdoors and after coming back home.
- If bitten, tick should be removed softly with the aid of tweezers.
- Use insect repellents containing DEET on your skin and clothes.
- Since DEET is toxic for our body, natural repellents made from plants such as lemongrass, rosemary and thyme essential oils can be used to ward off ticks.

How can Lyme disease be treated?
Treatment in all stages of Lyme disease is possible with short course of oral antibiotics such as doxycycline, amoxicillin, or azithromycin5. In chronic and more complicated cases of Lyme disease, three to four weeks of antibiotic therapy may be needed. Antibiotics should be used only after the diagnosis of Lyme disease is confirmed and should not be used prophylactically.
Since Lyme disease does not always appear in its typical presentation, the diagnosis is delayed. In absence of prompt treatment, chronic disease sets in causing serious complications such as cognitive impairment. Bacteria have become refractory to treatment due to excessive use of antibiotics in various stages of Lyme disease. In the wake of ever increasing antibiotic resistance, there is a strong need of alternative therapy which may be safe and effective.
References
- Rosenberg R. et al. Vital Signs: Trends in Reported Vectorborne Disease Cases — United States and Territories, 2004–2016. MMWR. CDC.May 2018;vol.67,no.17.
- Hinckley AF, Connally NP, Meek JI, et al. Lyme disease testing by large commercial laboratories in the United States. Clin Infect Dis. 2014;59(5):676-81.[Pubmed]
- Nau R, Christen HJ, Eiffert H. Lyme disease – current state of knowledge. Dtsch Arztebl Int. 2009;106:72–81
- Current Efforts in Lyme Disease Research. National Institute of Allergy and Infectious Diseases(NIAID), 2017
- Biesiada G, Czepiel J, Leśniak MR, Garlicki A, Mach T. Lyme disease: review. Arch Med Sci. 2012;8(6):978-82.







I was very pleased to find this web-site.I wanted to thanks for your time for this wonderful read!! I definitely enjoying every little bit of it and I have you bookmarked to check out new stuff you blog post.
That’s a very inspiring comment..thankyou!